 Single-incision laparoscopic inguinal hernia repair with or without... | Download Scientific Diagram
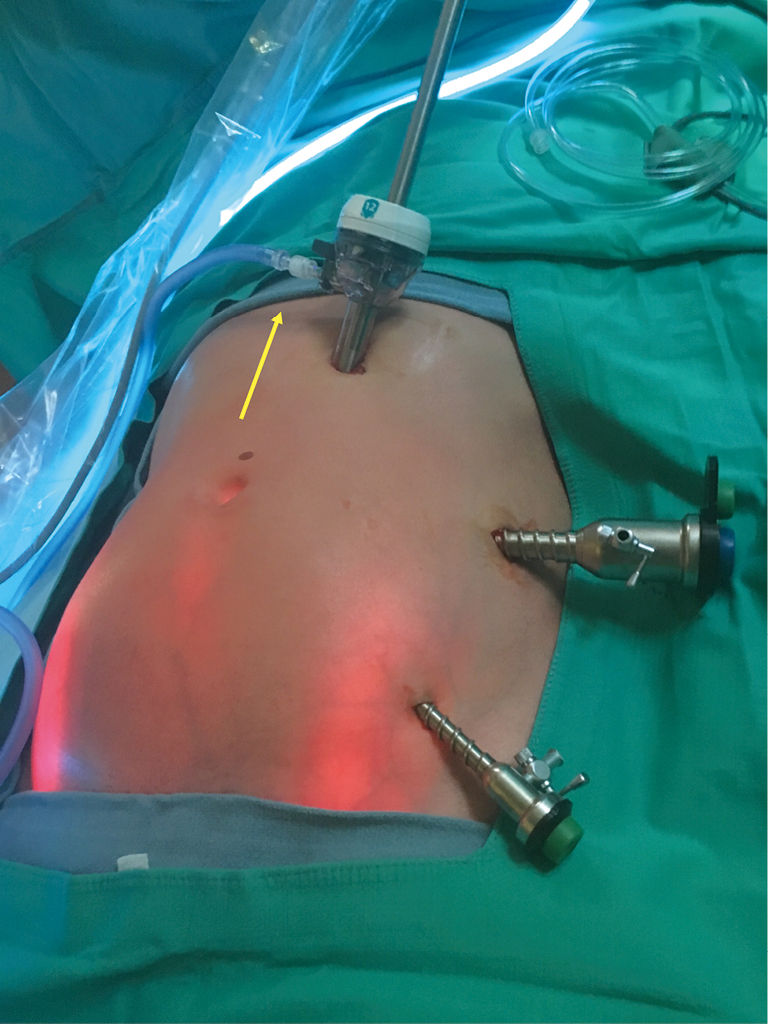
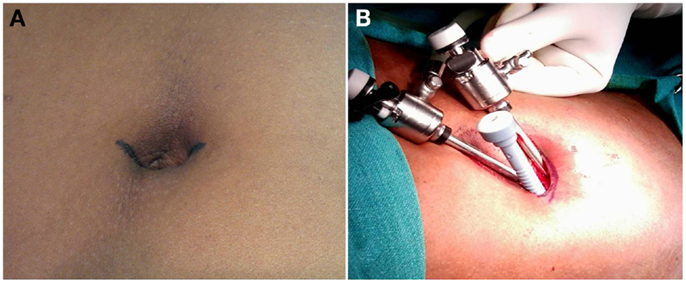
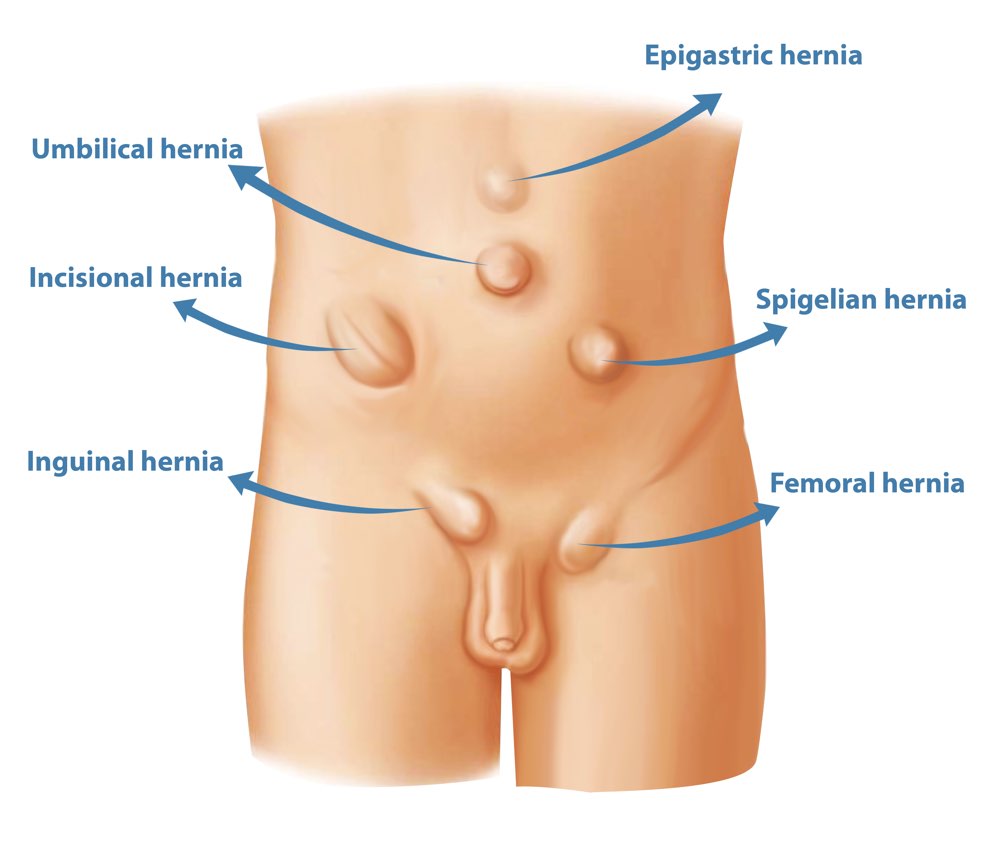
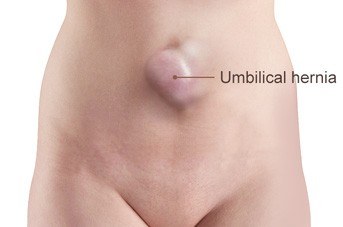
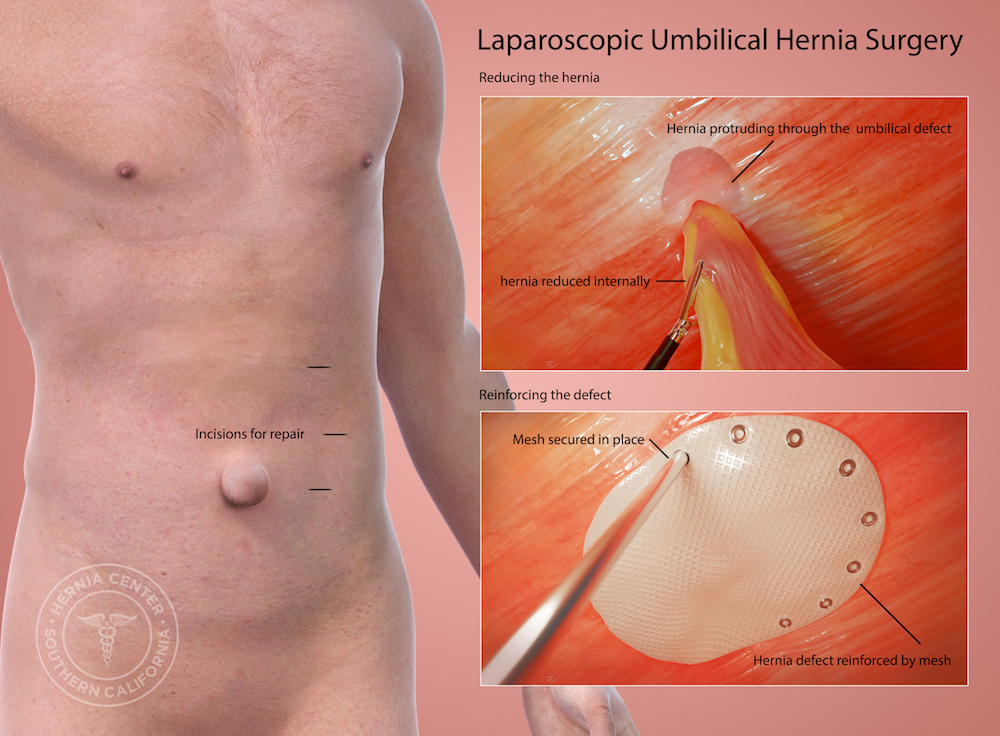
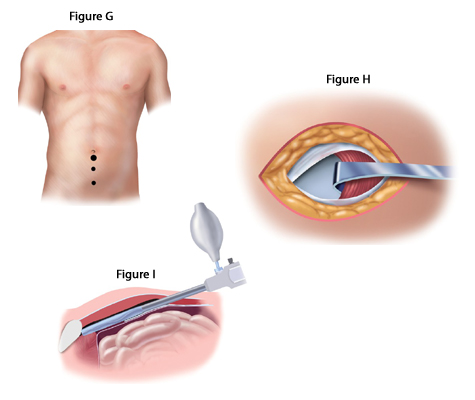
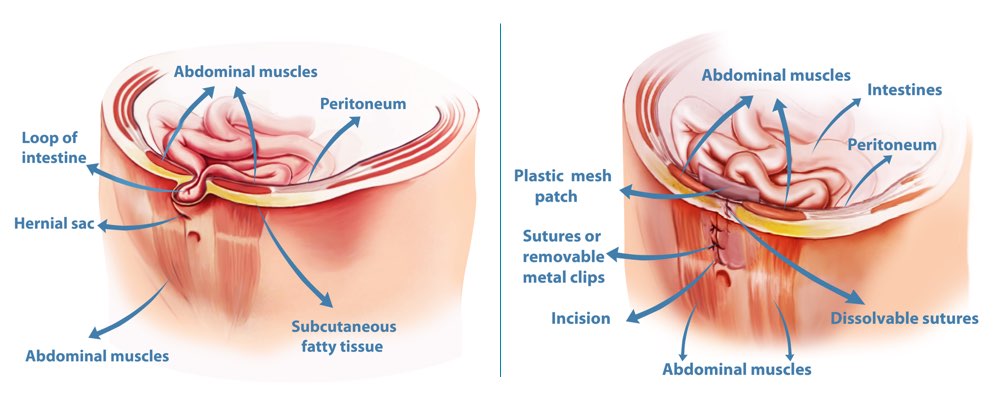
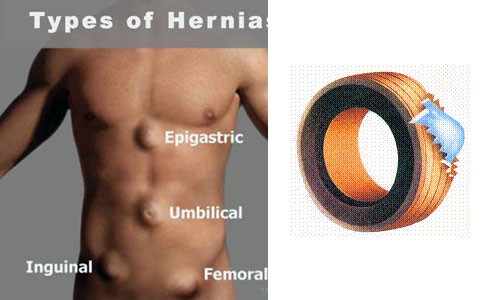
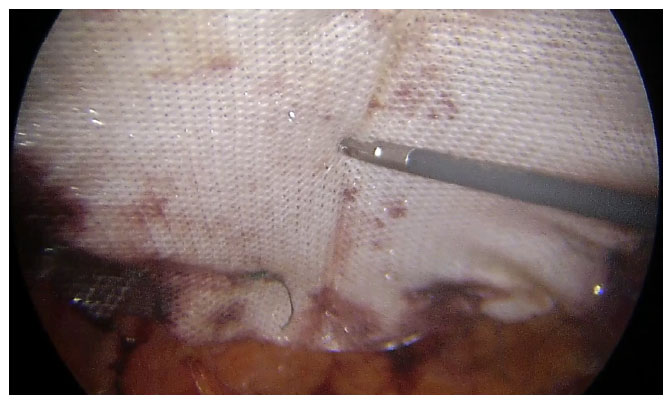
Single-incision laparoscopic inguinal hernia repair with or without... | Download Scientific DiagramInternational Scholarly Research Notices On this pageClinical study Silence Open AccessV. Abhishek, M. N. Mallikarjuna, B. S. Shivaswamy, "Laparoscopic Umbilical Hernia Repair: Technique Paper", International Scholarly Research Notices, vol. 2012, Article ID 906405, 4 pages, 2012. https://doi.org/10.5402/2012/906405Laparoscopic Reparation of Hernia Ubilical: Tapa Técnica V. Abhishek1Department of General Surgery, Hospital Victoria, Instituto de Medicina de Bangalore e Investigación, 128 Colonia de Médicos Vijay, Bangalore 560002, India2Konanakunte Bangalore, Karna. The repair of laparoscopic umbilical hernia has largely replaced the open method. The purpose of this study was to document the repair of laparoscopic umbilical hernia using two ports, herniorriafia combined with intraabdominal mesh fixing with transabdominal absorbable technique and to demonstrate that it is feasible, efficient and safe. Methods. Thirty-two patients with umbilical hernia were subjected to laparoscopic repair by combined herniorriafia and intraabdominal mesh. The technique of two ports was used and the umbilical defect was closed by transabdominal suture PDS, polypropylene and PTFE mesh was placed intra-bdominal and fixed to the abdominal wall by transabdominal suture PDS. Results. Thirty-two patients were subjected to laparoscopic repair. The operating time ranged from 45 min to 100 min (media 64 min). Early postoperative complication was observed in five patients with two who had ileum for 4 days and one patient each developed urinary retention, wound infection and seroma. The late postoperative complication was observed in 6 patients with five persistent abdominal pain complaints that were resolved without treatment and a case of keloids in port sites. None of the patients developed chronic pain or had recurrence during the follow-up period. Conclusion. Hernia umbilical laparoscopic repair with herniorriafia combined and intraabdominal mesh fixing by absorbable sutures offers efficient, safe and effective repair for hernia umbilical.1. Introduction As with hernia inguinal, the repair of hernia umbilical has undergone several developments with laparoscopic repair of hernia umbilical (LRUH) is gaining growing popularity due to its low rate of recurrence, short hospital stay and low complication rate []. The inguinal evaluation of hernia's repair of the result of the surgeries has gradually changed from recurrence to the development of chronic pain. With the laparoscopic repair of hernia ventral and incisional becoming the standard treatment care has gradually shifted to chronic pain as a result to compare various methods. Some issues should be addressed in the setting of LRUH of the prosthesis with monochrome or double helical lockers and transabdominal sutures (TAS), number of required ports, formation of seroma, incidence and management of chronic pain. This article reports our experience with the repair of laparoscopic umbilical hernia with the modification of the current procedure to address the above topics.2. Method From February 2009 to July 2011, 32 consecutive patients were subjected to an attempt to repair laparoscopic umbilical hernia using herniorriafia with mesh repair technique and were prospectively studied. The exclusion criteria were very large hernias and severe conditions conspicuous with high risk of general anesthesia. This series represents the experience with this technique for a single consulting surgeon. The patient is placed in the supine position with the left arm adjusted next to the patient. The monitors are placed on both sides of the bed's foot. A first-generation cephalosporin is given intravenously. After the general endotracheal anesthesia is induced, the abdominal skin is sterilized and enveloped. An orogástric tube is placed for stomach decompression. A pneumoperitoneum is achieved with a needle insert of Veress; the most preferred site for initial access is the Palmer point, a point 3 cm below the left rib margin in the midclavicular line, since it is less likely that you will find intraabdominal adhesions at this point []. Alternative sites include the right hypochondria and the right and left iliac fose. A 10 mm port is percutaneously placed on a point along the previous axillary line. An additional 5 mm port is placed under direct vision on the left side of the abdomen. A 30° laparoscope is placed through the port of 10 mm. A laparoscopic examination of the abdomen is performed and anomalies are observed. If there is no contraindication to proceed, the imprisoned content is reduced. This can be achieved with a combination of blunt and sharp dissection with scissors. Occasionally, the harmonic scale is useful if the adhesions are particularly vascular. You're not trying to remove the hernia sack. The abdominal wall is inspected for additional hernias. If none is found, the facial umbilical defect is carved by passing a transabdominal spinal needle. It is easy to overestimate the size of the defect when there is neupoperitoneum; therefore, the pressure of insufficiulation should be reduced to 8 to 10 mmHg for this step. The subsurface of the abdominal wall is cleaned from any fatty deposit that inhibits the smooth flat application of the mesh. A 2-5 mm incision is placed within the umbilical skin fold depending on the defect size. A suture step instrument like the Carter-thomason/Gore device was used for the umbilical defect closure. Using the device, and under direct vision, the PDS suture was introduced into the abdominal cavity on one side of the defect and recovered again on the other side of the defect after passing once again the suture step instrument. At least 3 sutures were placed through facial defect, and the sutures were then tied. The suture knots were buried under the skin, and the incision was closed with a subcutaneous suture. This technique, previously described by Carter [] for the closure of the troupe sites, is relatively easy to perform. The technique is no different from that involving the closure of the 10 mm ports and adds no more than 5 minutes to 10 minutes to the procedure. A suitable size mesh is chosen to properly close the defect with a 3 cm overlap circumferentially. We use the Proceed dual-layer mesh (ETHICON Johnson-Johnson), but many others are available. It is important to have 3 to 5 cm superimposed above all facial defect. Four polydiaxonesulphate 2-0 (PDS) sutures placed across the mesh polypropylene side in the corners. These are tied to the mesh with three square knots. The mesh is rolled and inserted through the port of 10 mm in the abdominal cavity. The larger pieces of mesh require the removal of the port and placement directly through the opening of the skin. The mesh is not inscribed inside the abdomen and placed with the side of the polypropylene against the abdominal wall and the side of the polytetrafluoroethylene downwards to the abdominal content. The pneumoperitoneum is decreased again at 10 mmHg and with a suture instrument, the corresponding suture pairs are stripped transabdominally through properly placed 2 mm skin incisions. The sutures are tight, and the mesh rises to the abdominal wall. A 3 to 5 cm flap is confirmed once again, and anchor sutures are tied in subcutaneous tissues. Additional sutures were placed if any mesh bounces were found. Tackers were not used for the subsequent fixing of the mesh. Pneumoperitoneum was released and the ports were closed. 3. Results Thirty-two patients were subjected to repair of laparoscopic umbilical hernia, twenty-five were women and seven men. The average age was 44 years (from 28 to 63 years). Two hernias involved the divarication of the recti muscles. The average defect size was 10 cm2 (range 1 cm2 to 24 cm2). The average size of the mesh was 110 cm2 (range 32 cm2 to 225 cm2). Twenty-six of them were operated with two-port techniques 6 patients required additional port, 4 because of dense adhesions it was difficult to spread the content of hernia sac, and 2 required additional 3rd port due to the difficulty of developing the large intraabdominal mesh. Operating time ranged from 45 min to 100 min (average 64 min). The average stay in the hospital was 2.6 days (from 2 to 7 days). The monitoring of the complications and recurrence of hernia was performed at an outpatient clinic of the sixth week and by telephone conversation every 6 months. The average follow-up period was 26.5 months. Eight patients were lost in follow-up from 5 to 12 months and 3 to 18 months, as they could not be contacted for phone interviews using the available contact details. There were no early complications (4 wk) in six (18.7%). Five (15.6%) patients complained of abdominal pain that resolved for 2-4 months without further treatment. A (3.1%) patient developed keloids at the post site and at the transabdominal suture fixation sites. Patients with chronic pain or recurrence during the follow-up period are not present. 4. Debate In laparoscopic technique, the mesh is placed in an intraperitoneal location and less often in the preperitoneal location, where the increase in intraabdominal pressures is completely spread throughout each square inch of the mesh and not along a line of dim suture, as happens in conventional suture repairs. An increase in intraabdominal pressures thus helps to keep the mesh in place instead of moving it, as is the case with conventional overlay repairs. The laparoscopic approach allows the surgeon to clearly and definitively define the margins of the hernia defect and identify additional defects that have not been clinically apparent previously. One of the key determinants of a high rate of recurrence after conventional repairs is the phenomenon of hidden hernias. These are the hernias that can be lost during an open repair. Finally, it is because a wide overlap of the malle defect would help to prevent intraabdominal forces from shifting the mesh to the defect. The laparoscopic approach allows easier placement of a larger prosthesis with good overlap. In the open approach, reaching a overlap of 3 to 5 cm requires extensive dissection of soft tissue, with the consequent increase of wound complications. This advantage is more prominent in obese patients and those with greater defects. The preferred mesh fixing method during laparoscopic umbilical hernia is controversial. The physics of mesh fixing during the repair of laparoscopic ventral hernia does not support the unique placement of tacks/other fixing devices. Most of the meshes used for the repair of laparoscopic umbilical hernia are approximately 1 mm thick and the spiral lockers are 4 mm long and occupy a profile of 1 mm on the surface of the patch. It can be expected that a perfectly placed locker will penetrate only 2 mm beyond the mesh; therefore, the tacks will probably not give the same grip force as a full thickness abdominal wall suture. Because many candidates who present for the repair of laparoscopic umbilical hernia are obese (with a substantial amount of preperitoneal fat), the penetration of 2 mm of the taca will not reach fascia in most cases. Experimental studies have confirmed the upper strength of sutures against tacks only in the fixing of mesh to the abdominal wall [, ]. They have concluded that the fixing of the mesh suture in the repair of laparoscopic umbilical hernia is essential, especially during the early period of mesh incorporation. Many proponents of the use of transabdominal sutures cite lower recurrence rates due to increased tensile resistance of sutures compared to tacks []. Other authors argue that the use of tacks significantly reduces surgical time by maintaining similar recurrence rates []. Recently, it has been shown that Mesh fixing with Fibrin Sealant in LUHR was associated with less acute postoperative pain, discomfort and a shorter convalence than fixing the lock or transabdominal suture without compromising the recurrence rate []. Many studies using the laparoscopic approach have reported a 10% recurrence rate [, ]. Mechanisms of recurrence of umbilical hernia described in the literature, in decreasing order of frequency are the infection, lateral detachment of the mesh, inadequate fixing of mesh, inadequate mesh, inadequate overlap, lost hernias, growing intraabdominal pressure, and trauma []. We note that the combined technique of herniorriafia with intraabdominal mesh in the repair of hernia umbilical reduced the possibilities of recurrence to the minimum. Seroma formation is not unique to the laparoscopic approach. Most seroma develop over the mesh and inside the hernial sac retained. The seroma formation rate in reported series varies depending on when the researchers evaluated it. The average incidence of seroma at 4 to 8 weeks is 11.4% in large reported series. In the largest multi-institutional trial, the seroma that was clinically apparent more than 8 weeks postoperatively was considered a complication and occurred in 2.6% cases []. Seroma incidences are greater where the mesh is fixed by the simple or double crown technique where the hernial defect is not erased. To reduce this we adopt the closing technique of the port site developed by Carter to close the umbilical defect or at least reduce the defect size using absorbable suture. Regardless of whether they are aspirated under sterile conditions or allowed to resolve, seroma rarely results in long-term problems. The aspiration for the seroma is recommended to be enlarged or persisted before reaching large sizes, when they can rarely result in the skin necrosis that is overheating. Patients should be advised preoperatively regarding the possibility of seroma formation after laparoscopic repair. Some authors argue that the use of tacks significantly reduces postoperative pain. Pain is usually worse after repair with sutures than with socks. The sutures penetrate through the full thickness of musculature and fascia of the abdominal wall. This has been theorized to cause local muscle ischemia leading to postoperative severe pain []. Cobb et al. [] has also proposed that intercostal nerves may enter transabdominal sutures causing chronic and persistent neuropathic pain. A series of repairs by transfascial sutures report persistent pain and discomfort in 1% to 6% of patients []. None of our patients presented persistent pain beyond 6 months. We prefer to use synthetic absorbable PDS for the fixing of mesh and the closure of umbilical defects, as these provide adequate fixation until the growth of the fibrous tissue in the mesh and also prevent the long-term accidental penetration of the nerves in sutures. Most authors feel that oral anti-inflammatory drugs or injections of local anesthesia may relieve symptoms in most cases []. Others have reported re-explorations for persistent pain, finding immediate relief after release of a suture from the site of symptoms []. The usual technique of 3 ports for the repair of hernia ventral is being replaced by technique of 2 ports [] and of a single port with time and similar operating results. It was observed that the 2-port technique was suitable for the dissection of content and sacred adhesions in cases of difficulty; additional ports can be used. The causes of postoperative morbidity, apart from those mentioned above, are unrecognized enterotomy, wound infection, intestinal obstruction by intraperitoneal abscess due to adherence to the disease and respiratory insufficiency. These complications often increase the hospital stay and the cost of treatment; however, the frequency of these complications is comparable to open technique []. There are encouraging results in comparative studies on the cost analysis of laparoscopic versus open repair of ventral hernias. In a recent series, the laparoscopic umbilical hernia repaired by a dual-layer polypropylene mesh and transfascial sutures significantly reduced the surgical infections of the site, the duration of the hospital stay and the costs compared to the repair of open mesh []. However, the types of mesh used and the fixing device can make considerable differences in cost calculations. We use transabdominal suture for mesh fixing with umbilical defect closure compared to tackers to reduce the cost of the procedure. 5. Conclusions Reparation of laparoscopic umbilical hernia with combined herniorrhaphy and intraabdominal mesh fixing by absorbable sutures offers the ideal result with low recurrence, and less complication of the formation of seroma of infection, and chronic pain with lower procedural cost. ReferencesCopyrightCopyright © 2012 V. Abhishek et al. This is an open access article distributed under the article, which allows unrestricted use, distribution and reproduction in any medium, provided that the original work is duly cited. More related articles Share Related articles
Accessibility links Search results Laparoscopic Hernia umbilical Repair: Technical PaperLaparoscopic Versus Open Umbilical Hernia ReparationLaparoscopic Umbilical / Paraumbilical Hernia Surgery, LondonAbstract versus mesh fixing in umbilical laparoscopic College ...A case of umbilical hernia imprisoned in an adult treated by ... current options in hernia umbilical repairs A complication to remember: next sinus point ...Mesh repair of laparoscopic umbilical hernia (IPOM Plus ...Reparation of umbilical hernia in cirrhotic patients: 18 ... Foot links

Umbilical Hernia Repair Dallas, TX | Keyhole Surgery Dallas, TX
Laparoscopic umbilical hernia repair surgery in Bangalore | Umbilical hernia repair, Hernia repair, Umbilical hernia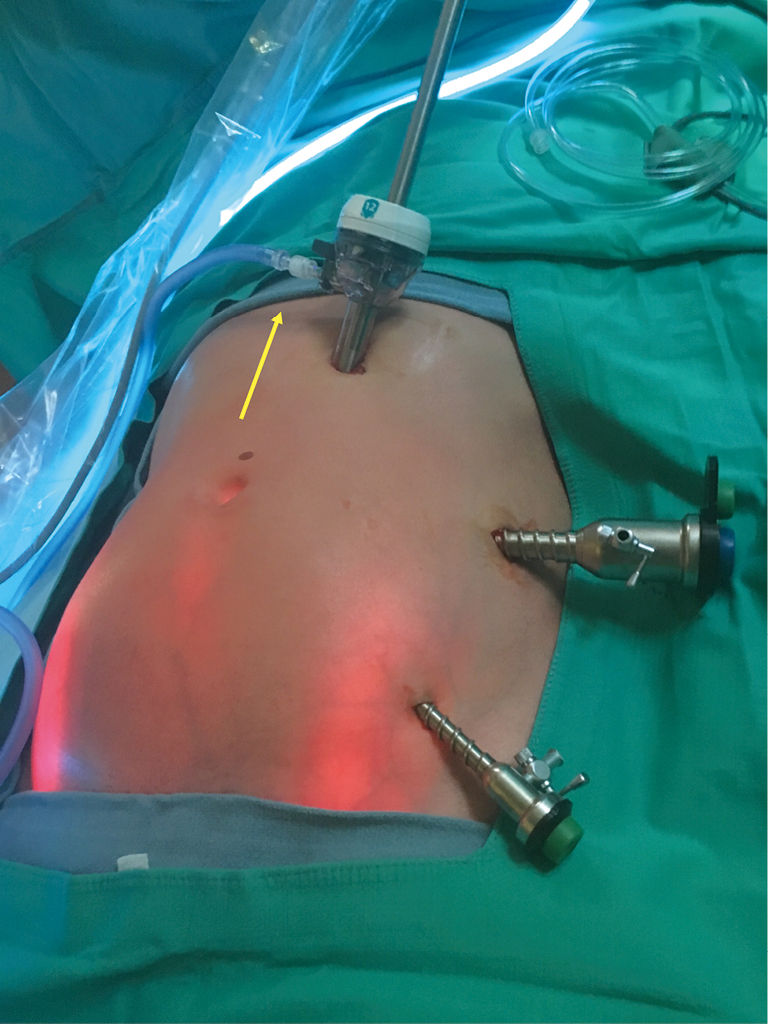
Laparoscopic umbilical herniorrhaphy: a novel technique of hernia neck closure and outcomes in the first 19 cases - Vetter - Laparoscopic Surgery
Umbilical hernia • MEDtube.net
Laparoscopic Repair of Umbilical Hernia - YouTube
Hernia Surgery | Chesapeake Vein Center & Medspa | Chesapeake, VA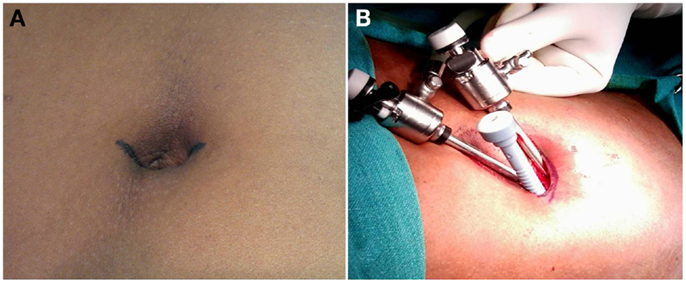
Frontiers | Minimal Incision Scar-Less Open Umbilical Hernia Repair in Adults – Technical Aspects and Short-Term Results | Surgery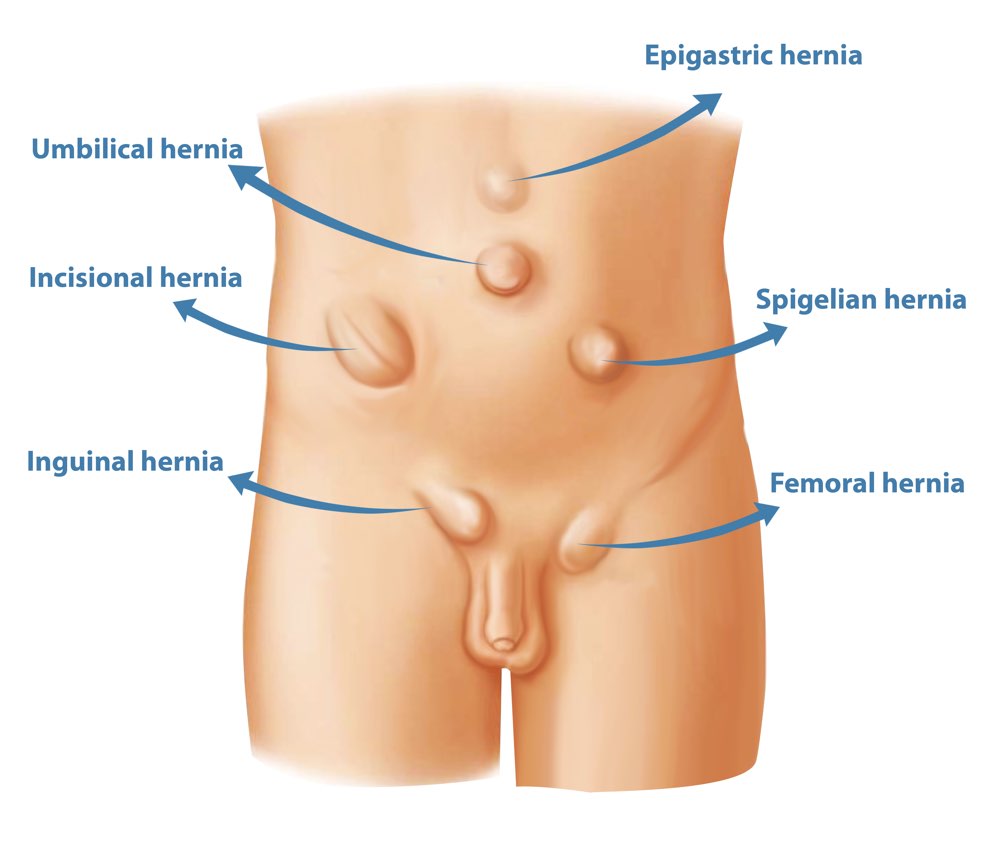
Types of Hernia | Hernia Surgery & Hernia Repair | Surgeons Perth
Needlescopic surgery for large umbilical hernia in a patient with morbid obesity using intraperitoneal onlay mesh with fascial defect closure: a case report | Surgical Case Reports | Full Text
Treatment | Premier Hernia Center
CSA Surgical Center - Belly Button (Umbilical) Hernia Repair
How Long Does It Take to Recover from an Umbilical Hernia Repair Surgery?
How to repair a small umbilical hernia laparoscopically - Matthews - 2020 - ANZ Journal of Surgery - Wiley Online Library
Internet Scientific Publications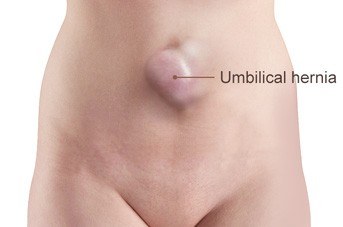
Umbilical Hernia Repair Melbourne | Keyhole Umbilical Hernia Repair Melbourne
Umbilical hernia: when and how - Maia - Annals of Laparoscopic and Endoscopic Surgery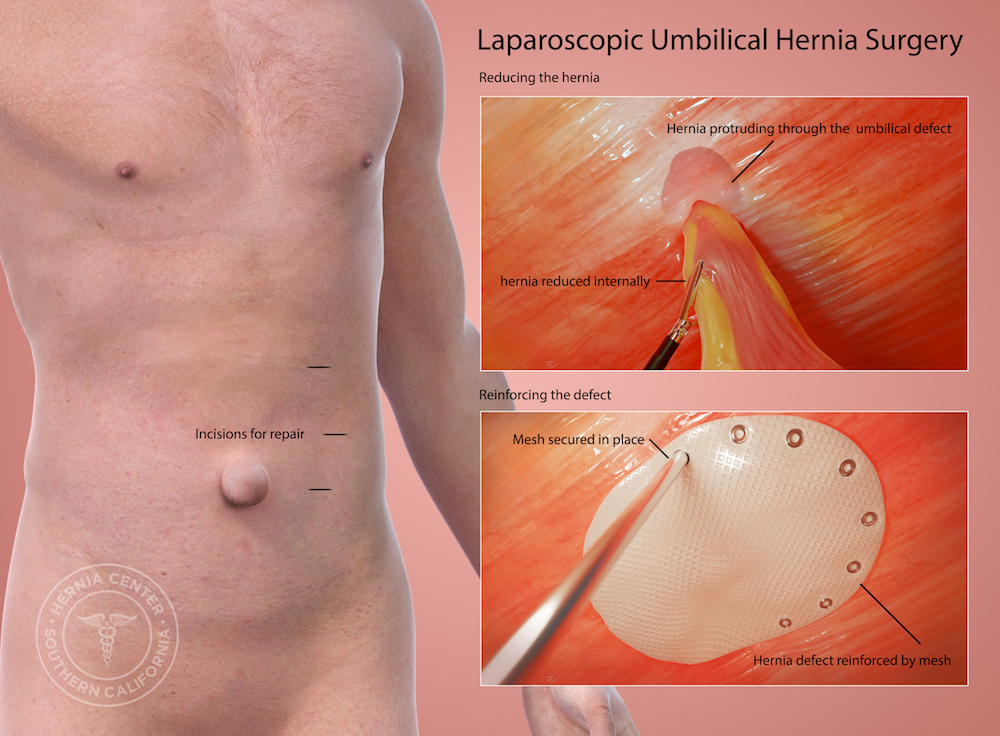
Umbilical Hernia Treatment Pasadena Orange County Riverside CA
Hernia: Types, Treatments, Symptoms, Causes & Prevention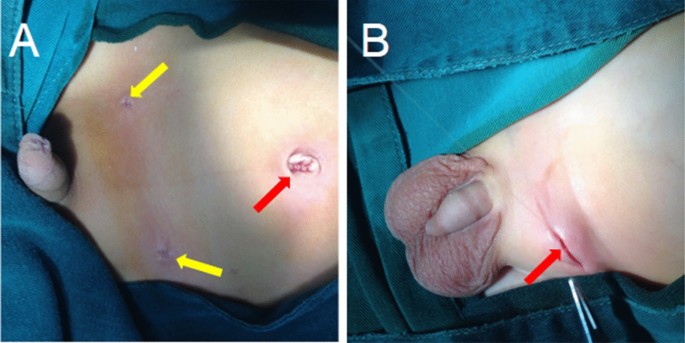
A comparative study examining laparoscopic and open inguinal hernia repair in children: a retrospective study from a single center in China | BMC Surgery | Full Text:max_bytes(150000):strip_icc()/hernia-surgery-in-detail-3157226_FINAL-ab113759eb27456b827498ca8db5c99b.png)
Hernia Repair Surgery: Overview
Laparascopic Incisional or Umbilical Hernia Surgery Patient Information, Ahmedabad - YouTube
Laparoscopic repair of complicated umbilical hernia with Strattice Laparoscopic™ reconstructive tissue matrix - ScienceDirect
Case 2: laparoscopic view of small bowel adhesions to the anterior... | Download Scientific Diagram
The pros and cons of laparoscopic surgery vs. open surgery for hernia repair
What to Expect During Umbilical Hernia Surgery Recovery - RELENTLESS FORWARD COMMOTION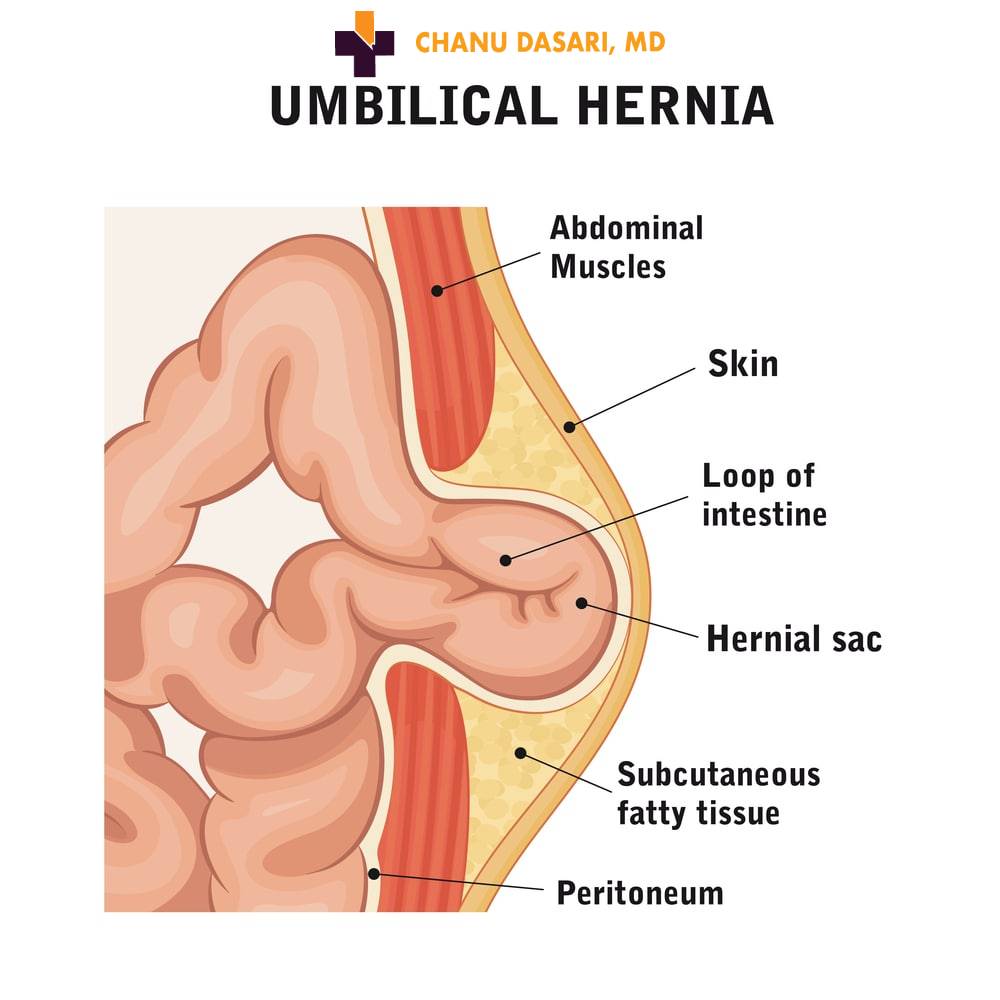
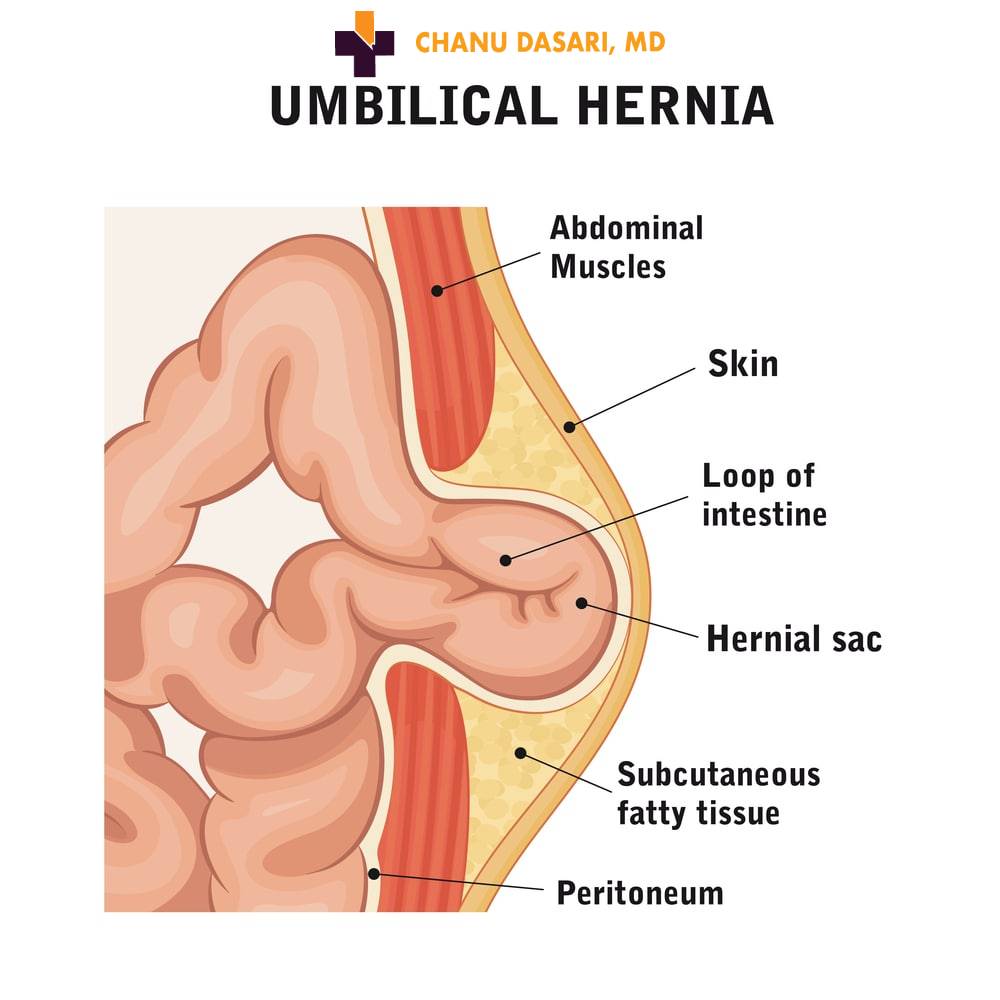
Umbilical Hernia | Best General Surgeon Dr. Chanu Dasari
Melbourne Hernia Surgery Centre | Laparoscopic, Robotic Hernia Surgery & Open Hernia Repair Surgery. Simple & Complex Hernia. - MR STEVEN KARAMETOS
Umbilical Hernia Repair Reviews | Was it Worth It? | RealSelf
Hernia Types - Umbilical - California Hernia Specialists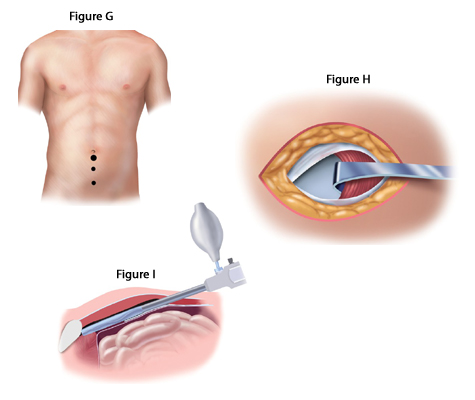
About Laparoscopic Hernia Surgery - California Hernia Specialists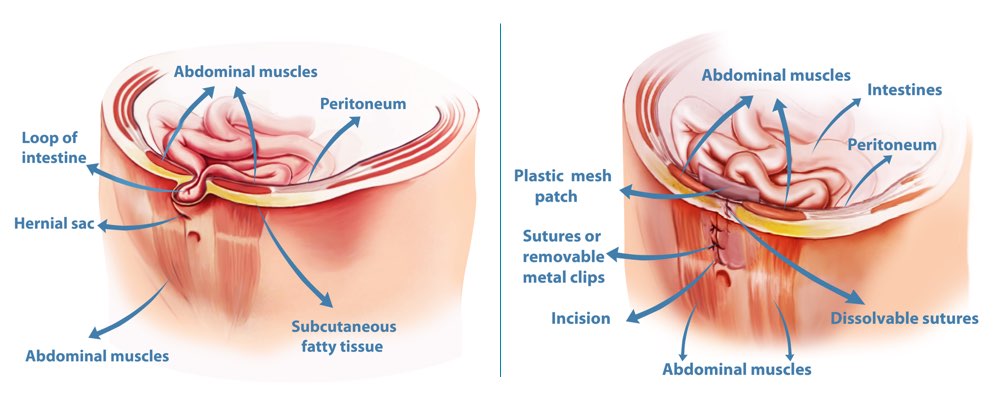
Hernia Repair Surgery Perth | Surgical Treatment for Hernias
Video: Laparoscopic Repair of Small Umbilical Hernia without Mesh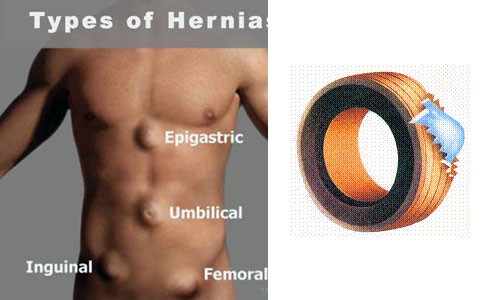
Hernia Laparoscopic Surgery Cost, Hernia Treatment
6-minutes laparoscopic surgery for umbilical hernia. What is better? - YouTube
Laparoscopic Hernia Repair High Res Stock Images | Shutterstock
Recovery After Hernia Repair: What to Expect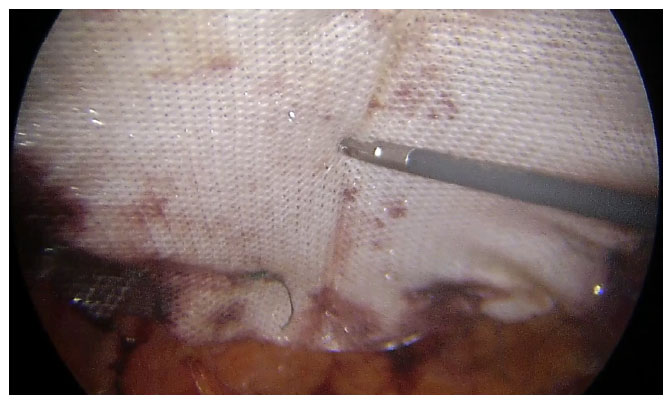
Laparoscopic intra-peritoneal onlay mesh plus repair for ventral abdominal wall hernias - is there substance to the hype?
Umbilical Hernia Repair Laparoscopic Umbilical Hernia Surgery | Umbilical hernia, Hernia repair, Umbilical hernia repair
Umbilical hernia: Causes, symptoms, and treatments
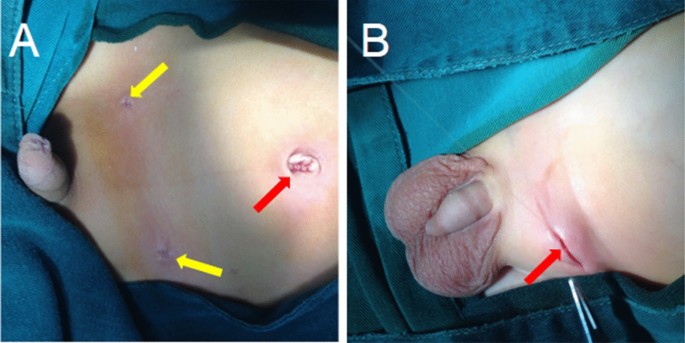
Transumbilical repair of umbilical hernia in children: The covert scar approach - Journal of Pediatric Surgery
 Single-incision laparoscopic inguinal hernia repair with or without... | Download Scientific Diagram
Single-incision laparoscopic inguinal hernia repair with or without... | Download Scientific Diagram











:max_bytes(150000):strip_icc()/hernia-surgery-in-detail-3157226_FINAL-ab113759eb27456b827498ca8db5c99b.png)











Posting Komentar untuk "laparoscopic umbilical hernia repair"